Safety of drugs in the elderly population in Italy
In recent years, the concept of deprescribing has been introduced, based on the reduction of the number of drugs taken in order to optimize the risk-benefit ratio of polypharmacy taking into account the goals of treatment and the preferences of the patient; however, the available intervention strategies are not numerous.1
Deprescribing is one of the issues addressed in the National Report on the use of drugs in the elderly population in Italy,2] produced in collaboration between the Istituto Superiore di Sanità (ISS) and Italian Medicine Agency (AIFA), which describes some local experiences of deprescribing carried out in different care settings.
The experience in nursing homes
A first experience concerns nursing homes. These facilities host elderly with chronic diseases, often treated with numerous psychotropic drugs3 that should be suspended to improve cognitive and functional performance.4 The experience, conducted in 10 nursing homes in Northern Italy in 2013-2014, concerned the identification of potentially inappropriate drugs in the institutionalized elderly (psychotropic: antipsychotics, antidepressants and benzodiazepines) and the subsequent modification of the prescription with the use of a software (INTERCheck). Results (272 participants) showed a reduction in the average number of medications (from 7.0±2.9 to 5.9±2.6) and in the percentage of subjects treated with psychotropic medications (-11.5%). Antipsychotics used for behavioural disorders in patients with dementia were reduced by 5.2%, benzodiazepines by 5.9%, and selective serotonin reuptake inhibitors by 8.1%. Thanks to this deprescribing intervention and the multidisciplinary approach that improved polypharmacy in the elderly, the percentage of subjects exposed to at least one potentially serious drug interaction was reduced (-21.3%) and there was no increase in adverse drug reactions.
The experience in hospital
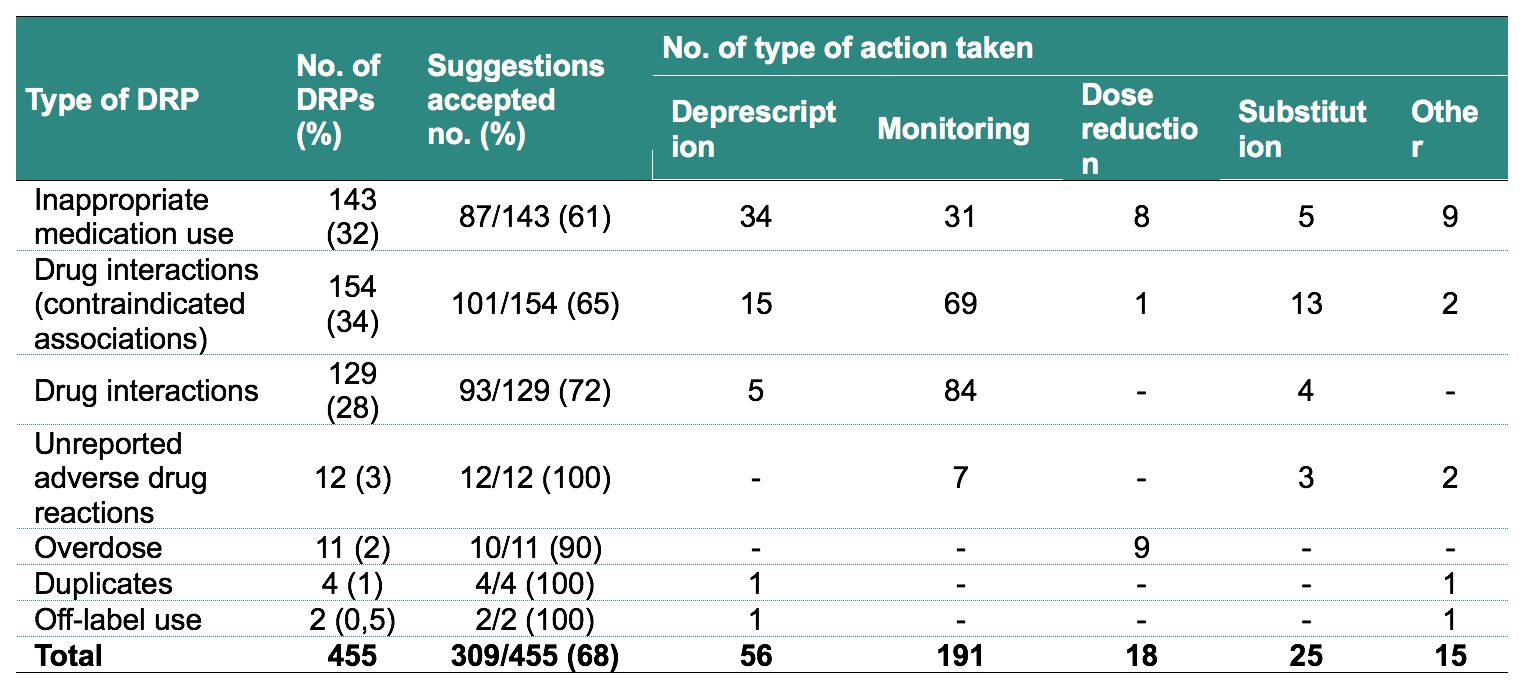
Multidisciplinary interventions are found in the experience of deprescribing in the elderly hospitalized patient, where the hospital pharmacist also participates in the management of therapy during hospitalization. A study, conducted at Polyclinic of Milan in 6 departments of Internal Medicine and Geriatrics, evaluated the effect of recognition-reconciliation-revision therapy (RRRT) on prescribing choices. The pharmacist, going within 24-72 hours from the entrance of the patient in hospital, carried out the RRRT intervention through the use of various tools (including the software INTERCheck-WEB3, developed by Mario Negri Pharmacological Research Institute), identifying potentially inappropriate drugs taken before admission, the possible occurrence of adverse drug reactions not reported and treatments not supported by real therapeutic needs. Everything was discussed with the physician, who chose whether to modify therapy. At discharge, after a new RRRT, a form was completed for the general practitioner to support the new therapeutic choices. Over the 12 months of the study, each ward enrolled 15 patients aged ≥75 years, chronically treated with at least 5 medications and a life expectancy >6 months. On average, 9.4 (±3.7) medications were taken during the inpatient stay, and 455 Drug-Related Problems (DRPs) were identified, 5 per patient, which mainly involved the prescribing of inappropriate medications and/or those at risk for serious interactions (Table 1). Deprescribing (n=56) was the most frequent action following the reporting of a drug-related problem.
Table 1. Number and types of drug-related problems (DRPs) identified as part of the therapeutic reconciliation-review process and actions taken by the physician after discussion with the pharmacist2
The experience in general practice
The use of platforms to support prescribing5 and the shared approach of therapeutic remodulation, have led to a reduction of various drug-related problems in the elderly hospitalized. These interventions also support general practitioners who, for continuity of care, should ensure the monitoring of patients’ therapies, also taking into account psycho-physical changes that may modify the overall benefit/risk ratio of therapies.
In this setting, in order to analyze deprescribing, an ad hoc study was conducted on the use of statins for the primary prevention of cerebro-cardiovascular events in elderly patients who do not benefit from such treatments6 through the analysis of data from the Health Search database of the Italian Society of General Medicine and Primary Care (SIMG). Among 9,568 patients aged over 80 years (without history of cardiovascular events), 20% were deprescribed statins. This intervention was similar between men and women but increased with age (31% in patients aged ≥90 years), also showed a geographical variability (deprescribing more in the North of Italy, 21%, than in the Centre, 18%, and in the South, 17%).
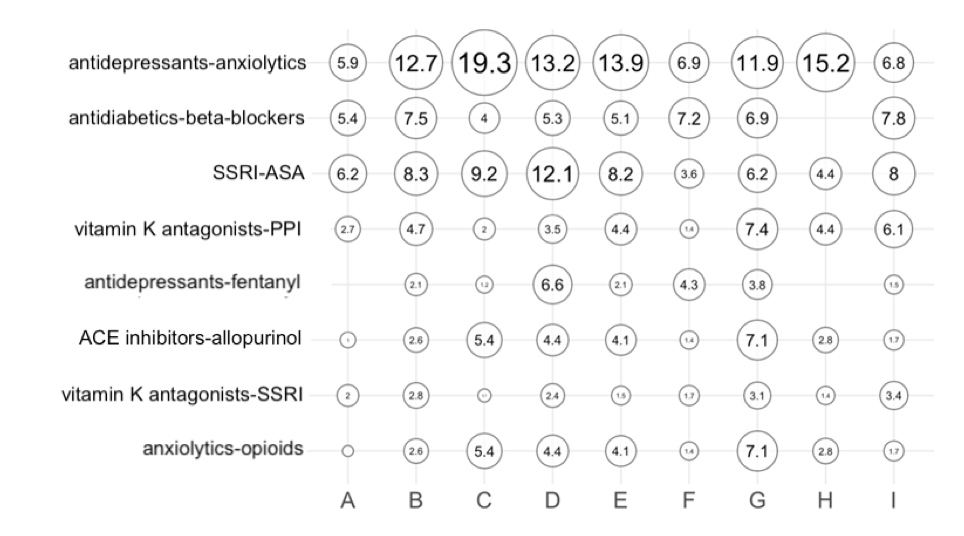
Deprescribing interventions are based on criteria of inappropriateness of medication use that allow limiting prescriptions of high risk drugs for the elderly.7,8 In a 2017-2018 study involving general practitioners and nursing homes from 9 Local Health Authorities in Emilia-Romagna Region, first indicators of inappropriateness most adequate to the context were identified, then measured and evaluated on the use of prescribed medications. Following clinical audits, post-intervention changes were assessed with a focus on drug interactions that, especially in nursing homes, were very frequent during the pre-intervention phase (Figure 1). There were decreases in the prevalence of simultaneous use of at least 10 drugs (6%), inappropriate prescriptions of proton pump inhibitors (20%), and benzodiazepines taken chronically (10%). At the territorial level, cases of non-adherence to statins, antidepressants and bisphosphonates were reduced (by 30%, 14% and 6% respectively). About 30% of patients had at least one combination, among the 159 considered, of drugs at risk of interaction: corrective interventions led to a 10% decrease.
Figure 1. Pre-intervention analysis: prevalence of potential drug interactions in nursing homes of different Local Health Authorities2
Individual Local Health Authorities are represented by a letter. The numbers within the bubbles represent the prevalence as a percentage of patients observed
SSRI: selective serotonin reuptake inhibitors
ASA: acetylsalicylic acid
PPI: proton pump inhibitors
In practice
The National Report2 describes some experiences of deprescribing based on the sharing of methods and activities to achieve defined and measurable objectives, useful to direct clinicians towards a better appropriateness of use of drugs in the elderly. Deprescribing represents an action of primary importance to be carried out in the various care settings and, starting from local experiences, should be extended to the whole national territory. The achievement of this objective should then be maintained through monitoring with a high degree of quality of prescriptions and optimal standards of care in the elderly.
Ilaria Ippoliti1, Graziano Onder2, Roberto Da Cas1, Luca Pellizzari3, Paola Ruggeri1
1 National Center for Research and Preclinical and Clinical Evaluation of Drugs, Istituto Superiore di Sanità (ISS)
2 Department of Cardiovascular, Endocrine-Metabolic Diseases and Aging, Istituto Superiore di Sanità (ISS)
3 Geriatrics A, Verona Integrated University Hospital
- Jansen J, Naganathan V, et al. Too much medicine in older people? Deprescribing through shared decision making. BMJ 2016;353:i2893
- Osservatorio Nazionale sull’impiego dei Medicinali. L’uso dei farmaci nella popolazione anziana in Italia. Rapporto Nazionale 2019. Roma, Agenzia Italiana del Farmaco, 2021. https://www.aifa.gov.it/documents/20142/1577699/OsMed_Farmaci_anziani_13...
- Cioltan H, Alshehri S, et al. Variation in use of antipsychotic medications in nursing homes in the United States: a systematic review. BMC Geriatr 2017;17(1):32.
- Gedde M, Husebo B, et al. Less is more: the impact of deprescribing psychotropic drugs on behavioral and psychological symptoms and daily functioning in nursing home patients. Results from the cluster-randomized controlled COSMOS trial. Am J Geriatr Psychiatry 2020;29:304-15.
- Riduzione della politerapia negli anziani attraverso l’uso di uno strumento elettronico di supporto decisionale: i risultati italiani di uno studio controllato randomizzato multicentrico europeo. Osservatorio Nazionale sull’impiego dei Medicinali. L’uso dei farmaci nella popolazione anziana in Italia. Rapporto Nazionale 2019. Roma, Agenzia Italiana del Farmaco, 2021
- Van der Ploeg M, Floriani C, et al. recommendations for (discontinuation of) statin treatment in older adults: review of guidelines. J Am Geriatr Soc 2020;68:417-25.
- By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2019;67:674-94.
- O’Mahony D, O’Sullivan D, et al. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing 2015;44:213-8.